Understanding Diabetes: Causes, Symptoms, and Essential Precautions to Stay Healthy
by admin Science & Nature
Diabetes is a chronic disease that occurs when the pancreas does not produce enough insulin or when the body cannot effectively use the insulin it produces. Insulin is a hormone that regulates blood glucose. It affects millions globally, and understanding it is key to living a healthy life.Think of your body like a finely tuned engine, and glucose, a type of sugar is its primary fuel. This glucose comes from the food you eat. Now, imagine a vital component of this engine, insulin, acting as a key that unlocks your cells, allowing glucose to enter and provide energy.
In diabetes, this system malfunctions. There are two main types you might have heard of: Type 1 diabetes and Type 2 diabetes. The main cause of diabetes varies by type. But no matter what type of diabetes you have, it can lead to excess sugar in the blood. Too much sugar in the blood can lead to serious health problems.
TYPES OF DIABETES

Chronic diabetes: conditions include type 1 diabetes and type 2 diabetes.
Potentially reversible diabetes conditions include: prediabetes and gestational diabetes. Prediabetes happens when blood sugar levels are higher than normal. But the blood sugar levels aren't high enough to be called diabetes. And prediabetes can lead to diabetes unless steps are taken to prevent it. Gestational diabetes happens during pregnancy. But it may go away after the baby is born.
Type 1 Diabetes: The Body's Immune System Misstep
With Type 1 diabetes, the body's immune system mistakenly attacks and destroys the beta cells in the pancreas that produce insulin. It's like a friendly fire incident within your body. As a result, your pancreas produces little to no insulin. People with Type 1 diabetes need to take insulin daily, usually through injections or an insulin pump, to survive. It's often diagnosed in children and young adults, and while the exact cause isn't fully understood, genetics and environmental factors likely play a role. Think of it as an absolute insulin deficiency.
Type 2 Diabetes: Insulin Resistance and Relative Deficiency
Type 2 diabetes is far more common. In this case, your body either doesn't produce enough insulin or the cells become resistant to the insulin that is produced. Imagine the locks on your cells becoming rusty and difficult for the insulin key to open. This is called insulin resistance. Over time, the pancreas may also struggle to keep up with the demand for more insulin, leading to a relative insulin deficiency.
Several factors increase the risk of developing Type 2 diabetes, including:
- Weight: Excess weight, particularly around the abdomen, can make cells more resistant to insulin.
- Family History: Having a close relative with Type 2 diabetes increases your risk.
- Physical Inactivity: Regular exercise helps your body use glucose more efficiently.
- Age: The risk increases as you get older.
- Ethnicity: Certain ethnicities have a higher predisposition
- Prediabetes: This is a condition where blood sugar levels are higher than normal but not yet high enough to be diagnosed as Type 2 diabetes. It's a critical window for intervention!
The Ripple Effects: Complications of Diabetes.
Uncontrolled diabetes can lead to serious health problems, affecting various parts of the body. Think of high blood sugar as a corrosive substance circulating in your bloodstream over time. Some potential complications include:
Heart Disease and Stroke: Diabetes significantly increases the risk of these cardiovascular issues.
Kidney Disease (Diabetic Nephropathy): High blood sugar can damage the filtering units in the kidneys.
Nerve Damage (Diabetic Neuropathy): This can cause numbness, tingling, and pain, especially in the feet and legs.
Eye Damage (Diabetic Retinopathy): High blood sugar can damage the blood vessels in the retina, potentially leading to blindness.
Foot Problems: Nerve damage and poor circulation can lead to serious foot infections and even amputation.
The Empowering Path: Managing Diabetes
While diabetes is a chronic condition, it can be effectively managed! The key is a proactive approach involving:
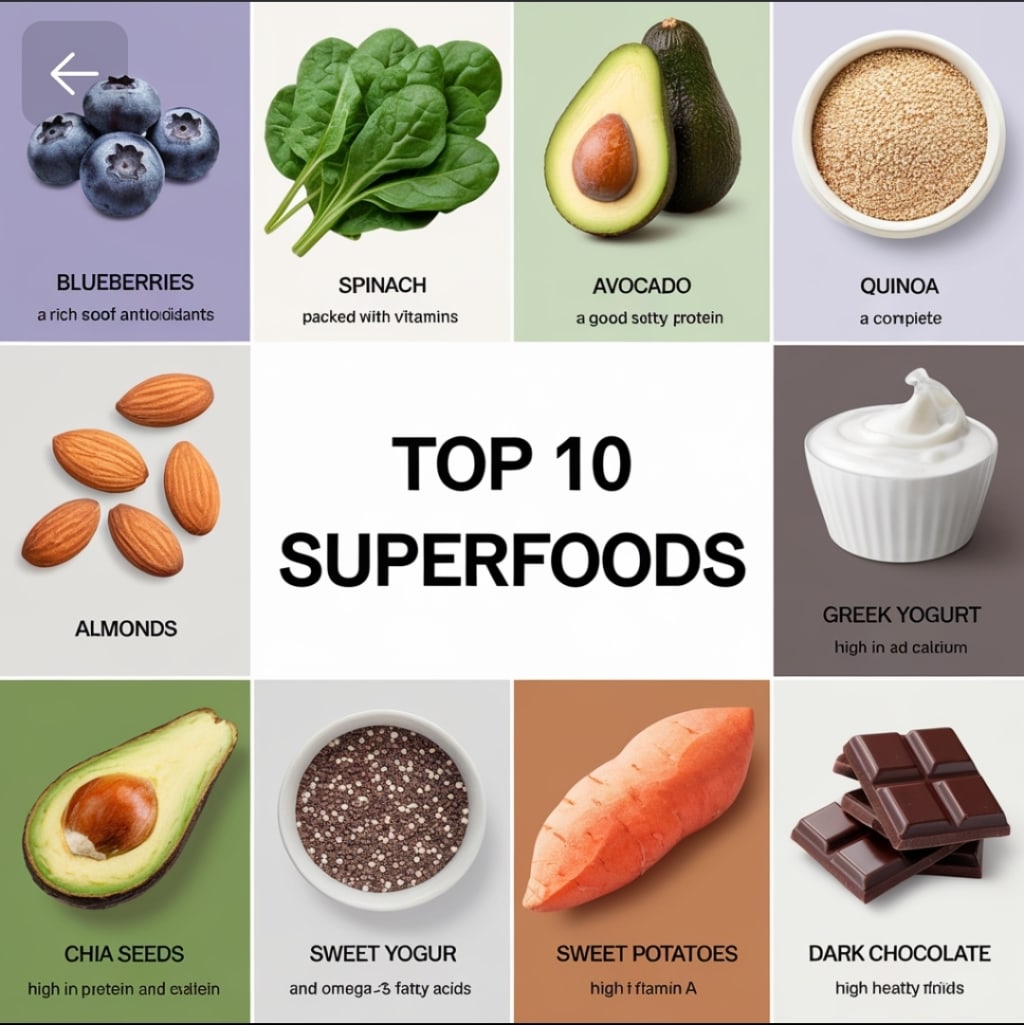
Healthy Eating: Focusing on whole foods, fruits, vegetables, and lean protein while limiting sugary drinks and processed foods is crucial for blood sugar control.
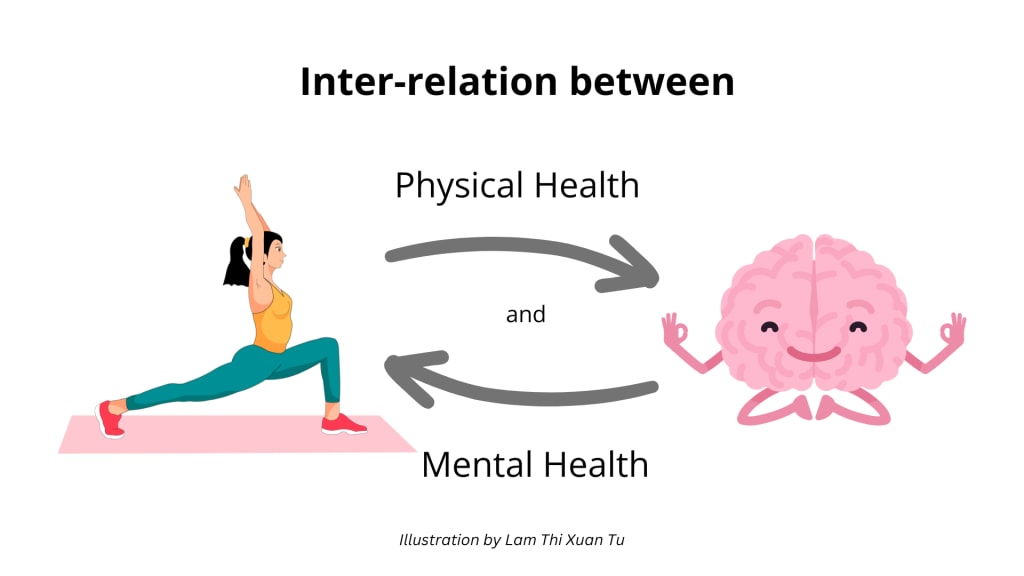
Regular Exercise: Physical activity helps improve insulin sensitivity and manage weight.
Medication: People with Type 1 diabetes need insulin. Many individuals with Type 2 diabetes may also require oral medications or injectable medications, including insulin, to help regulate blood sugar levels.
Sugar Monitoring: Regularly checking blood sugar levels with a glucose meter or continuous glucose monitor (CGM) provides valuable information for making informed decisions about diet, exercise, and medication.
Regular Checkups: Working closely with your healthcare team, including doctors, dietitians, and diabetes educators, is essential for managing the condition and preventing complications.
What happens if my blood glucose level becomes too high?
High blood glucose is called hyperglycemia. Symptoms that your blood glucose levels may be too high include:
- Feeling thirsty
- Feeling tired or weak
- Headaches
- Urinating (peeing) often
- Blurred vision
If you often have high blood glucose levels or symptoms of high blood glucose, talk with your healthcare team. You may need a change in your diabetes meal plan, physical activity plan, or diabetes medicines.
High blood glucose may also be caused by other conditions that can affect insulin or glucose levels in your blood. These conditions include problems with your pancreas or adrenal glands.
What happens if my blood glucose level becomes low for me?
Hypoglycemia, also called low blood glucose, happens when your blood glucose level drops below what is healthy for you. For many people with diabetes, this means a blood glucose reading lower than 70 mg/dL. Your number might be different, so check with your healthcare team to find out what blood glucose level is low for you.
Symptoms of low blood glucose tend to come on quickly. The symptoms can be different for everyone, but they may include:
- Shaking
- Sweating
- Nervousness or anxiety
- Irritability or confusion
- Feeling dizzy
- Hunger
Low blood glucose levels can be common in people with Type 1 diabetes and people with type 2 diabetes who take certain diabetes medicines. If you think you may have low blood glucose, check your level, even if you don't have symptoms. Low blood glucose can be dangerous and should be treated as soon as possible.
Although it's rare, you can still get low blood glucose without having diabetes. The causes can include conditions such as liver disease, kidney disease, and hormone deficiencies (lack of certain hormones). Some medicines, such as certain heart medicines and antibiotics, can also cause it. See your provider to find out the cause of your low blood glucose and how to treat it.
CONCLUSION.
Living with diabetes requires commitment and knowledge. Understanding the different types, risk factors, potential complications, and management strategies empower individuals to take control of their health and live full, active lives. It's not about limitations; it's about making informed choices and embracing a lifestyle that supports well-being. Remember, you are not alone, and with the right tools and support, you can navigate the journey of diabetes successfully.
When to see a doctor
If you think you or your child may have diabetes. If you notice any possible diabetes symptoms, contact your healthcare provider. The earlier the condition is diagnosed, the sooner treatment can begin.
If you've already been diagnosed with diabetes. After you receive your diagnosis, you'll need close medical follow-up until your blood sugar levels stabilize.
share with

Mesha M. Founder
"Explore a world of inspiration and empowerment at RealtimeArticles. Dive into our curated articles for insights, reflection, and shared growth. Join our community on a journey of discovery and evolution!"



Comments
Coming Soon!
POST YOUR COMMENTS